LVLUP Health
Ultimate GI Repair
Ultimate GI Repair
Approximately 320.34 AUD
Couldn't load pickup availability
Ultimate GI Repair
The most powerful gastrointestinal tract healing product in the world!
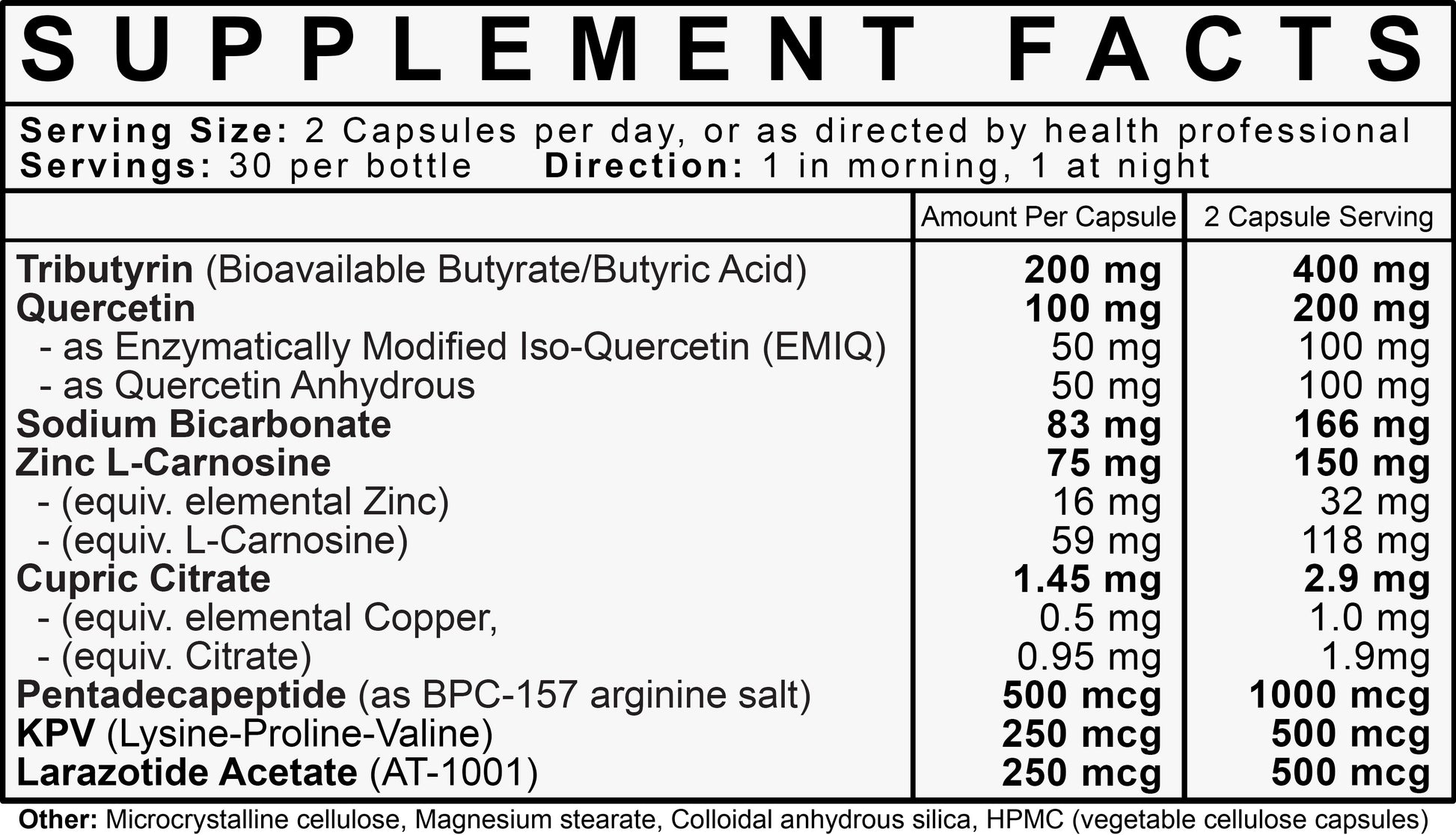
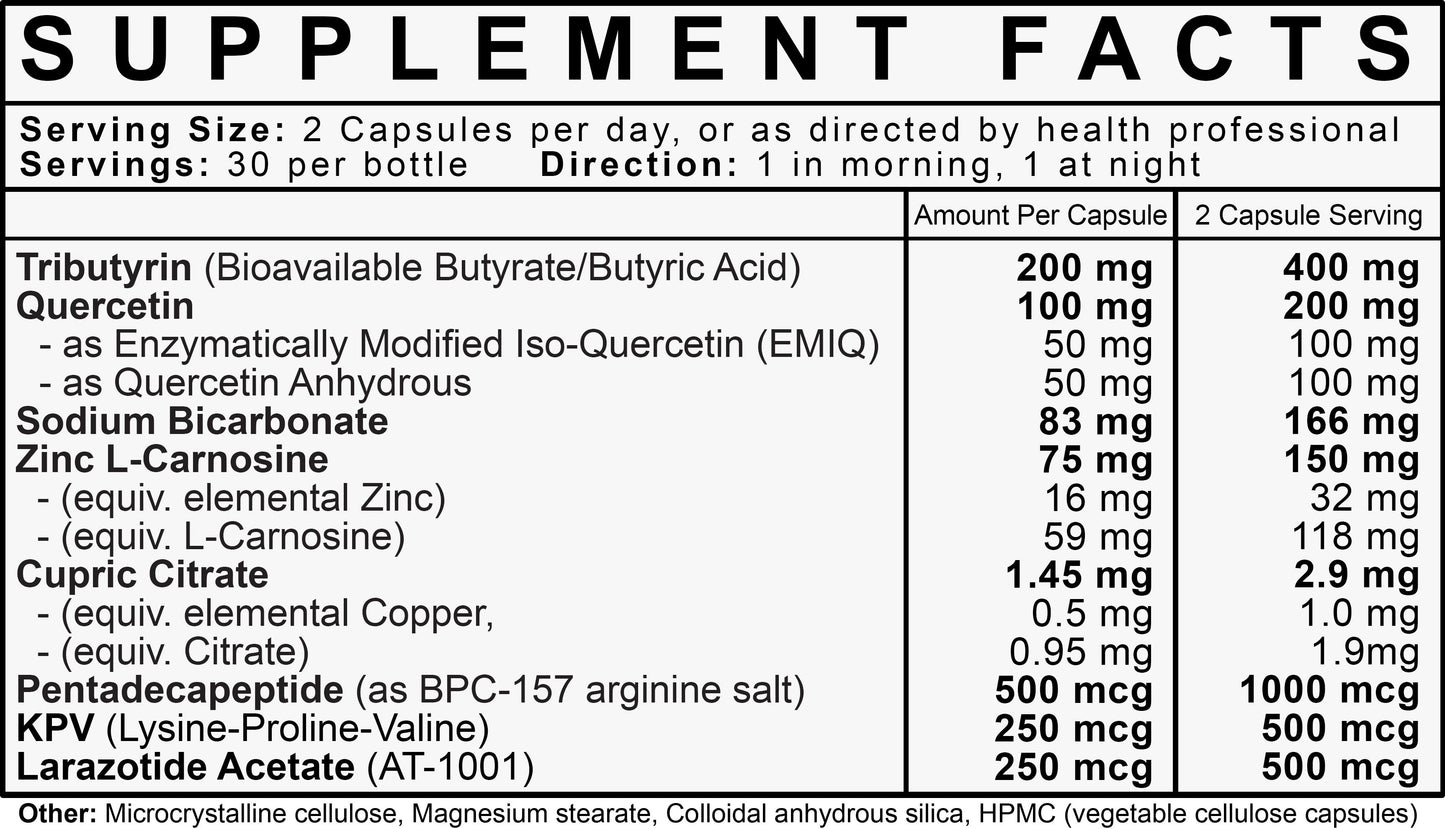
Combining 3 orally active peptides; BPC-157 (as Arginine salt), Larazotide Acetate (AT1001), KPV Tripeptide, with gut healing naturals, Zinc L-Carnosine, Quercetin (EMIQ for increased absorption), Tributyrin (the best, most bioavailable form of butyrate) Copper (to balance out the high dose of zinc), and Sodium Bicarbonate (stomach acidity buffer to increase peptide absorption).
Why is Ultimate GI Repair so pricey?
Why is Ultimate GI Repair so pricey?
There is no denying that Ultimate GI Repair is on the pricier end.
This is due to the compounds used within Ultimate GI Repair and their difficulty of sourcing and manufacturing.
We do hope however to reduce the price as the compounds become more readily available in the future.That being said even though the price is much higher than many other gut healing supplements it is not something people need to take long term.In fact most people need it for only 1 – 2 months at most to see noticeable results.Which makes it a lot more cost effective in the long run instead of taking a supplements for 12 months or even years.
How long before I see results?
How long before I see results?
Our customers typically see results within 1 month of taking the product.
Do I need to keep taking Ultimate GI?
Do I need to keep taking Ultimate GI?
Ultimate GI has been created to help speed up the process of healing.
It is not something that was intended or needs to be taken long term.
We recommend customers cycle the product by taking it for 1 month and if they still haven’t seen noticeable improvements an additional month and then breaking from it before cycling it again as needed.
Dosing Instructions
Dosing Instructions
Take one capsule twice daily away from food or as directed by health professional. (and not with enzyme supplements)
Note: High dose zinc may cause stomach upset, nausea or vomiting for some people when taken away from food. If this happens take with food (carbs or fats best; taking with protein less ideal)

Joe Rogan, Ben Greenfield and Dave Asprey On BPC 157 (the Star Ingredient in Ultimate GI Repair)
Description
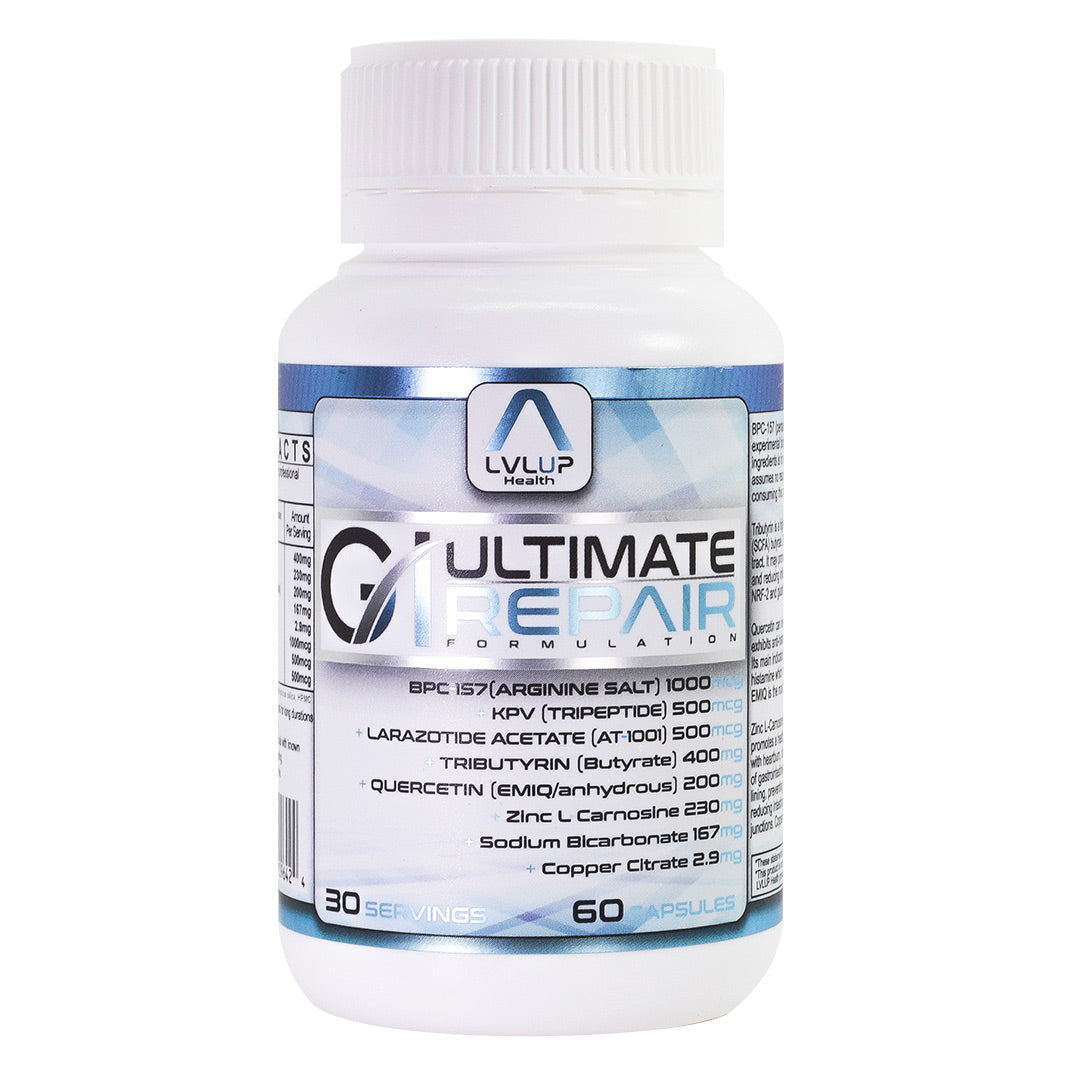
ULTIMATE GI REPAIR
A SYNERGISTIC combination of powerful peptides BPC-157, KPV, Larazotide Acetate,
and Naturals Zinc L-Caronsine, Quercetin (As EMIQ and Anhydrous), Tributyrin and Copper citrate to create THE most POWERFUL Gastro-Intestinal healing product on the market!
Each bottle contains 60 capsules; 30 serves.
Legal Disclaimer:*This product is intended for research purposes only. All productinformation available on the website is for educational purposes only.Bodily introduction of any kind into humans is done at the person’s ownrisk, and LVLUP Health assumes no responsibility for health outcomes,good or bad that may result from ingestion or use. Use should besupervised by a qualified healthcare professional.
Peptides
-
BPC-157
Learn More...– As highly absorbable form BPC157-Arginine
– Enhances injury and wound recovery– Heals the Gastro-Intestinal (GI) tract
– Stimulates blood vessel formation (angiogenesis)
– Upregulates Growth Hormone Receptors
– Enhances collagen production and formation
– Anti-Inflammatory
– Cytoprotective
-Modulates Nitric Oxide (NO)
– Reduces Neuroinflammation
-
LARAZOTIDE ACETATE
Learn more...– AT1001
– Zonulin Antagonist
– Decreases intestinal permeability.
– Prevents Tight Junction breakdown/disassembly
– The “Anti-Coeliac” peptide
– May reduce food sensitivity
– Immune modulating
– Reduces Neuroinflammation
*Mechanisms are based on preliminary study interpretations only.
Research and clinical trials are still being performed on this peptide. -
KPV
Learn more...- Aids in healing of injuries and wounds
- Potent Anti-Inflammatory
- Heal and enhance overall gut health
- Reduce pro-inflammatory cytokines
- Enhances collagen production and formation
- Improves skin health
- Strengthens Immune System
- Anti Microbial
- Cytoprotective
Naturals
-
Tributyrin
Learn more...– Best form of supplemental butyrate
– Increases mucus production
– Accelerates gastrointestinal wound healing
– Fuel source for the epithelium
– Maintains gastric mucosal barrier integrity.
– Reduces intestinal hyper-permeability
– Cytoprotective
– Stabilises mast cells (Antihistamine) -
Zinc L-Carnosine
Learn more...– Anti- inflammatory/ Antioxidant
– Accelerates gastrointestinal wound healing
– Anti-Ulcer
– Stimulate mucus production
– Maintains gastric mucosal barrier integrity.
– Reduces intestinal hyper-permeability
– Cytoprotective
– Stabilises mast cells (Antihistamine) -
Quercetin (2 forms)
Learn more...1) EMIQ (highly bioavailable systemic form)
2) Quercetin anhydrous (low absorption for local for GI effect)
–May help with Allergies and histamine– Blocks mast cells degranulation (Antihistamine)
– “Seals” the tight junction GI barrier
– Anti-Inflammatory/ Anti- Oxidant
– Cytoprotective
– May support heart health
– Immune Modulating
– Hepatoprotective (helps the liver)
-
Other
– Copper Citrate (For Zinc Copper ratio balancing); GI Repair contains a very high dose of Zinc, which needs to be balanced out by copper if used for a prolonged period of time.
– Sodium Bicarbonate (Acid buffer for increased peptide absorption)
-Bicarbonate buffers pepsinogen to pepsin conversion which needs low pH (high acidity) to occur.
Dosage Instructions

Take one capsule twice daily away from food, or as directed by health professional.
High dose zinc may cause stomach upset, nasaea or vomiting when taken away from food.
Do NOT take on an empty stomach if these symptoms occur, otherwise taking on an empty stomach is best.
Research
BPC 157
1. Butler, R. J., Marchesi, S., Royer, T., & Davis, I. S. (2007). Effective Therapy of Transected Quadriceps Muscle in Rat:Gastric Pentadecapeptide BPC 157. Journal of Orthopaedic Research September, 25(June), 1121–1127. https://doi.org/10.1002/jor
2. Brcic, L., Brcic, I., Staresinic, M., Novinscak, T., Sikiric, P., & Seiwerth, S. (2009). Modulatory effect of gastric pentadecapeptide BPC 157 on angiogenesis in muscle and tendon healing. Journal of Physiology and Pharmacology : An Official Journal of the Polish Physiological Society, 60 Suppl 7, 191–196.
3. Cerovecki, T., Bojanic, I., Brcic, L., Radic, B., Vukoja, I., Seiwerth, S., & Sikiric, P. (2010). Pentadecapeptide BPC 157 (PL 14736) improves ligament healing in the rat. Journal of Orthopaedic Research, 28(9), 1155–1161. https://doi.org/10.1002/jor.21107
4. Chang, C. H., Tsai, W. C., Hsu, Y. H., & Pang, J. H. S. (2014). Pentadecapeptide bpc 157 enhances the growth hormone receptor expression in tendon fibroblasts. Molecules, 19(11), 19066–19077. https://doi.org/10.3390/molecules191119066
5. Chang, C. H., Tsai, W. C., Lin, M. S., Hsu, Y. H., & Su Pang, J. H. (2011). The promoting effect of pentadecapeptide BPC 157 on tendon healing involves tendon outgrowth, cell survival, and cell migration. Journal of Applied Physiology, 110(3), 774–780. https://doi.org/10.1152/japplphysiol.00945.2010
6. Gjurasin, M., Miklic, P., Zupancic, B., Perovic, D., Zarkovic, K., Brcic, L., Sikiric, P. (2010). Peptide therapy with pentadecapeptide BPC 157 in traumatic nerve injury. Regulatory Peptides, 160(1–3), 33–41. https://doi.org/10.1016/j.regpep.2009.11.005
7. Gwyer, D., Wragg, N. M., & Wilson, S. L. (2019). Gastric pentadecapeptide body protection compound BPC 157 and its role in accelerating musculoskeletal soft tissue healing. Cell and Tissue Research, 377(2), 153–159. https://doi.org/10.1007/s00441-019-03016-8
8. Perovic, D., Kolenc, D., Bilic, V., Somun, N., Drmic, D., Elabjer, E., … Sikiric, P. (2019). Stable
gastric pentadecapeptide BPC 157 can improve the healing course of
spinal cord injury and lead to functional recovery in rats. Journal of Orthopaedic Surgery and Research, 14(1), 1–12. https://doi.org/10.1186/s13018-019-1242-6
9. Pevec, D., Novinscak, T., Brcic, L., Sipos, K., Jukic, I., Staresinic, M., … Sikiric, P. (2010). Impact of pentadecapeptide BPC 157 on muscle healing impaired by systemic corticosteroid application. Medical Science Monitor, 16(3), 81–88. https://pubmed.ncbi.nlm.nih.gov/20190676/
10. Seiwerth, S., Sikiric, P., Grabarevic, Z., Zoricic, I., Hanzevacki, M., Ljubanovic, D., … Kolega, Z. (1997). BPC 157’s effect on Healing. Journal of Physiology Paris, 91(3–5), 173–178. https://doi.org/10.1016/S0928-4257(97)89480-6
11. Sever, A. Z., Sever, M., Vidovic, T., Lojo, N., Kolenc, D., Vuletic, L. B., … Sikiric, P. (2019). Stable gastric pentadecapeptide BPC 157 in the therapy of the rats with bile duct ligation. European Journal of Pharmacology, 847(January), 130–142.
https://doi.org/10.1016/j.ejphar.2019.01.030
12. Sikiric, P. (1999). The pharmacological properties of the novel peptide BPC 157 (PL-10). Inflammopharmacology, 7(1), 1–14. https://doi.org/10.1007/s10787-999-0022-z
13. Sikirić, P., Petek, M., Ručman, R., Seiwerth, S., Grabarević, Z., Rotkvić, I., … Karakas, I. (1993). A new gastric juice peptide, BPC. An overview of the stomach-stress-organoprotection hypothesis and beneficial effects of BPC. Journal of Physiology – Paris, 87(5), 313–327. https://doi.org/10.1016/0928-4257(93)90038-U
14.
Sikiric, P., Seiwerth, S., Rucman, R., Kolenc, D., Vuletic, L. B.,
Drmic, D., Grgic, T., Strbe, S., Zukanovic, G., Crvenkovic, D.,
Madzarac, G., Rukavina, I., Sucic, M., Baric, M., Starcevic, N.,
Krstonijevic, Z., Bencic, M. L., Filipcic, I., Rokotov, D. S., &
Vlainic, J. (2016). Brain-gut Axis and Pentadecapeptide BPC 157: Theoretical and Practical Implications. Current neuropharmacology, 14(8), 857–865. https://doi.org/10.2174/1570159×13666160502153022
15. Staresinic, M., Sebecic, B., Patrlj, L., Jadrijevic, S., Suknaic, S., Perovic, D., … Sikiric, P. (2003). Gastric
pentadecapeptide BPC 157 accelerates healing of transected rat Achilles
tendon and in vitro stimulates tendocytes growth. Journal of Orthopaedic Research, 21(6), 976–983. https://doi.org/10.1016/S0736-0266(03)00110-4
LARAZOTIDE ACETATE
1.Gopalakrishnan, S., Tripathi, A., Tamiz, A. P., Alkan, S. S., & Pandey, N. B. (2012). Larazotide acetate promotes tight junction assembly in epithelial cells. Peptides, 35(1), 95–101. https://doi.org/10.1016/j.peptides.2012.02.016
2.
Gopalakrishnan, S., Durai, M., Kitchens, K., Tamiz, A. P., Somerville,
R., Ginski, M., Paterson, B. M., Murray, J. A., Verdu, E. F., Alkan, S.
S., & Pandey, N. B. (2012). Larazotide acetate regulates epithelial tight junctions in vitro and in vivo. Peptides, 35(1), 86–94. https://doi.org/10.1016/j.peptides.2012.02.015
3.
Kelly, C. P., Green, P. H., Murray, J. A., Dimarino, A., Colatrella,
A., Leffler, D. A., Alexander, T., Arsenescu, R., Leon, F., Jiang, J.
G., Arterburn, L. A., Paterson, B. M., Fedorak, R. N., & Larazotide
Acetate Celiac Disease Study Group (2013). Larazotide acetate in patients with coeliac disease undergoing a gluten challenge: a randomised placebo-controlled study. Alimentary pharmacology & therapeutics, 37(2), 252–262. https://doi.org/10.1111/apt.12147
4. Khaleghi, S., Ju, J. M., Lamba, A., & Murray, J. A. (2016). The potential utility of tight junction regulation in celiac disease: focus on larazotide acetate. Therapeutic advances in gastroenterology, 9(1), 37–49. https://doi.org/10.1177/1756283X15616576
5.
Leffler, D. A., Kelly, C. P., Abdallah, H. Z., Colatrella, A. M.,
Harris, L. A., Leon, F., Arterburn, L. A., Paterson, B. M., Lan, Z. H.,
& Murray, J. A. (2012). A randomized, double-blind study of larazotide acetate to prevent the activation of celiac disease during gluten challenge. The American journal of gastroenterology, 107(10), 1554–1562. https://doi.org/10.1038/ajg.2012.211
6. Serena, G., Kelly, C. P., & Fasano, A. (2019). Nondietary Therapies for Celiac Disease. Gastroenterology clinics of North America, 48(1), 145–163. https://doi.org/10.1016/j.gtc.2018.09.011
7. Valitutti, F., & Fasano, A. (2019). Breaking Down Barriers: How Understanding Celiac Disease Pathogenesis Informed the Development of Novel Treatments. Digestive diseases and sciences, 64(7), 1748–1758. https://doi.org/10.1007/s10620-019-05646-y
8. Yoosuf, S., & Makharia, G. K. (2019). Evolving Therapy for Celiac Disease. Frontiers in pediatrics, 7, 193. https://doi.org/10.3389/fped.2019.00193
KPV Tripeptide
In a mice model of colitis (colon inflammation), oral administration of KPV (added to drinking water) inhibited the activation of NF-κB and MAP kinase inflammatory signalling pathways and reduced pro-inflammatory cytokine secretion.
- Dalmasso G, Charrier-Hisamuddin L, Nguyen HT, Yan Y, Sitaraman S, Merlin D. PepT1-mediated tripeptide KPV uptake reduces intestinal inflammation. Gastroenterology. 2008;134(1):166–178. doi:10.1053/j.gastro.2007.10.026
KPV exerts its anti-inflammatory activities through inhibition of NF-kappaB translocation and activation of MC(1) receptor/cAMP.
- Mandrika I, Muceniece R, Wikberg JE. Effects of melanocortin peptides on lipopolysaccharide/interferon-gamma-induced NF-kappaB DNA binding and nitric oxide production in macrophage-like RAW 264.7 cells: evidence for dual mechanisms of action. BiochemPharmacol. 2001;61(5):613-21.
- Haddad JJ, Lauterbach R, Saadé NE, Safieh-garabedian B, Land SC. Alpha-melanocyte-related tripeptide, Lys-d-Pro-Val, ameliorates endotoxin-induced nuclear factor kappaB translocation and activation: evidence for involvement of an interleukin-1beta193-195 receptor antagonism in the alveolar epithelium. Biochem J. 2001;355(Pt 1):29-38.
In an animal model of colitis, KPV significantly reduced intestinal inflammation.
- Rajora N, Boccoli G, Catania A, et al. α-MSH modulates experimental inflammatory bowel disease. Peptides. 1997;18:381–385.
- Oktar BK, Ercan F, Ye en BC, et al. The effect of α-melanocyte stimulating hormone on colonic inflammation in the rat. Peptides. 2000;21:1271–1277.
KPV fights inflammation by inhibiting tumuor necrosis factor-α stimulated NF-κB activity and suppressing antigen-induced lymphocyte proliferation.
- Kelly JM, Moir AJ, Carlson K, et al. Immobilized α-melanocyte stimulating hormone 10–13 (GKPV) inhibits tumor necrosis factor-α stimulated NF-κB activity. Peptide. 2006;27:431–437.
-Cooper A, Robinson SJ, Pickard C, et al. α-melanocyte-stimulating hormone suppresses antigen-induced lymphocyte proliferation in humans independently of melanocortin 1 receptor gene status. J Immunol. 2005;175:4806–4813.
KPV suppresses inflammation through modulation of physiological responses in host defence.
-Hiltz ME, Lipton JM. Antiinflammatory activity of a COOH-terminal fragment of the neuropeptide alpha-MSH. FASEB J. 1989;3(11):2282-4.
KPV exhibits its anti-inflammatory effect through inhibition of IL-1beta functions.
-Getting SJ, Schioth HB, Perretti M. Dissection of the anti-inflammatory effect of the core and C-terminal (KPV) alpha-melanocyte-stimulating hormone peptides. J PharmacolExpTher. 2003;306(2):631-7.
KPV fights inflammation by stimulating cAMP generation in a concentration- dependent way.
-Schiöth HB, Muceniece R, Mutule I, Wikberg JE. New melanocortin 1 receptor binding motif based on the C-terminal sequence of alpha-melanocyte-stimulating hormone. Basic ClinPharmacolToxicol. 2006;99(4):287-93.
KPV combats inflammation by significantly inhibiting NF-kappaB activity.
- Kelly JM, Moir AJ, Carlson K, Yang Y, Macneil S, Haycock JW. Immobilized alpha-melanocyte stimulating hormone 10-13 (GKPV) inhibits tumor necrosis factor-alpha stimulated NF-kappaB activity. Peptides. 2006;27(2):431-7.
Several studies have shown a significant reduction of pro‐inflammatory substances such as IL1 β, IL6, TNFα, IL8, Groα, and interferon γ (IFNγ) following KPV treatment.
-Luger T A, Scholzen T, Grabbe S. The role of α‐melanocyte stimulating hormone in cutaneous biology. J Invest DermatolSympProc 1997287–93.
- Brzoska T, Luger TA, Maaser C, Abels C, Böhm M. Alpha-melanocyte-stimulating hormone and related tripeptides: biochemistry, antiinflammatory and protective effects in vitro and in vivo, and future perspectives for the treatment of immune-mediated inflammatory diseases. Endocr Rev. 2008;29(5):581-602.
In murine models of colitis, KPV treatment showed significant anti-inflammatory effects which suggests that it can be an important therapeutic option in treating inflammatory bowel disease.
- Klaus Kannengiesser, MD, et al. Melanocortin-derived tripeptide KPV has anti-inflammatory potential in murine models of inflammatory bowel disease, Inflammatory Bowel Diseases, Volume 14, Issue 3, 1 March 2008, Pages 324–331, https://doi.org/10.1002/ibd.20334.
In a mice model of ulcerative colitis, oral administration of KPV loaded into hyaluronic acid (HA)-functionalized polymeric nanoparticles (NPs) was effective in alleviating intestinal inflammation.
- Xiao B, Xu Z, Viennois E, Zhang Y, Zhang Z, Zhang M, Han MK, Kang Y, Merlin D. Orally Targeted Delivery of Tripeptide KPV via Hyaluronic Acid-Functionalized Nanoparticles Efficiently Alleviates Ulcerative Colitis. Mol Ther. 2017 Jul 5;25(7):1628-1640. doi: 10.1016/j.ymthe.2016.11.020. Epub 2017 Jan 28. PMID: 28143741; PMCID: PMC5498804.
ZINC L CARNOSINE
1. Hewlings, S., & Kalman, D. (2020). A Review of Zinc-L-Carnosine and Its Positive Effects on Oral Mucositis, Taste Disorders, and Gastrointestinal Disorders. Nutrients, 12(3), 665. https://doi.org/10.3390/nu12030665
2. Lyseng-Williamson, K.A. Zinc L-carnosine in gastric ulcers: a profile of its use. Drugs Ther Perspect 35, 463–469 (2019). https://doi.org/10.1007/s40267-019-00667-z
3. Mahmood, A., FitzGerald, A. J., Marchbank, T., Ntatsaki, E., Murray, D., Ghosh, S., & Playford, R. J. (2007). Zinc carnosine, a health food supplement that stabilises small bowel integrity and stimulates gut repair processes. Gut, 56(2), 168–175. https://doi.org/10.1136/gut.2006.099929
4. Miyoshi, A. Matsu, H et al. (1995). Clinical Evaluation of Zinc Carnosine in Treatment of Gastritis. http://www.citicam.net/moondance/pdf/4.pdf
5.
Odashima, M., Otaka, M., Jin, M., Wada, I., Horikawa, Y., Matsuhashi,
T., Ohba, R., Hatakeyama, N., Oyake, J., & Watanabe, S. (2006). Zinc
L-carnosine protects colonic mucosal injury through induction of heat
shock protein 72 and suppression of NF-kappaB activation. Life sciences, 79(24), 2245–2250. https://doi.org/10.1016/j.lfs.2006.07.032
6. Ooi, T. C., Chan, K. M., & Sharif, R. (2017). Antioxidant,
Anti-inflammatory, and Genomic Stability Enhancement Effects of Zinc
l-carnosine: A Potential Cancer Chemopreventive Agent?. Nutrition and cancer, 69(2), 201–210. https://doi.org/10.1080/01635581.2017.1265132
7. Sakae, K., Agata, T., Kamide, R. and Yanagisawa, H. (2013). Effects of L‐Carnosine and Its Zinc Complex (Polaprezinc) on Pressure Ulcer Healing. Nutrition in Clinical Practice, 28: 609-616. https://doi.org/10.1177/0884533613493333
8. Sharif, R., Thomas, P., Zalewski, P., Graham, R. D., & Fenech, M. (2011). The
effect of zinc sulphate and zinc carnosine on genome stability and
cytotoxicity in the WIL2-NS human lymphoblastoid cell line. Mutation research, 720(1-2), 22–33. https://doi.org/10.1016/j.mrgentox.2010.12.004
9. Sturniolo, G. C., Fries, W., Mazzon, E., Di Leo, V., Barollo, M., & D’inca, R. (2002). Effect of zinc supplementation on intestinal permeability in experimental colitis. The Journal of laboratory and clinical medicine, 139(5), 311–315. https://doi.org/10.1067/mlc.2002.123624
10. Sturniolo, G. C., Di Leo, V., Ferronato, A., D’Odorico, A., & D’Incà, R. (2001). Zinc supplementation tightens “leaky gut” in Crohn’s disease. Inflammatory bowel diseases, 7(2), 94–98. https://doi.org/10.1097/00054725-200105000-00003
QUERCETIN
1.
Bischoff, S. C., Barbara, G., Buurman, W., Ockhuizen, T., Schulzke, J.
D., Serino, M., Tilg, H., Watson, A., & Wells, J. M. (2014).
Intestinal permeability-a new target for disease prevention and therapy.
BMC gastroenterology, 14, 189. https://doi.org/10.1186/s12876-014-0189-7
2.
Graefe EU, Wittig J, Mueller S, Riethling AK, Uehleke B. (2001).
Pharmacokinetics and bioavailability of quercetin glycosides in humans.
Journal of Clinical Pharmacology. 41:492-499. http://ucce.ucdavis.edu/files/datastore/608-67.pdf
3.
Groschwitz KR, and Hogan SP. (2009). Intestinal barrier function:
molecular regulation and disease pathogenesis. Journal of Allergy and
Clinical Immunology. 124(1):3-20. https://www.ncbi.nlm.nih.gov/pubmed/19560575
4. Li Y, Yao J, Han C, Yang J, Chaudhry MT. (2016). Quercetin, inflammation, and immunity. Nutrients. 8(3):167. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4808895/
5.
Pearce, F. L., Befus, A. D., & Bienenstock, J. (1984). Mucosal mast
cells. III. Effect of quercetin and other flavonoids on antigen-induced
histamine secretion from rat intestinal mast cells. The Journal of allergy and clinical immunology, 73(6), 819–823. https://doi.org/10.1016/0091-6749(84)90453-6
6.
Salehi, B., Machin, L., Monzote, L., Sharifi-Rad, J., Ezzat, S. M.,
Salem, M. A., Merghany, R. M., El Mahdy, N. M., Kılıç, C. S., Sytar, O.,
Sharifi-Rad, M., Sharopov, F., Martins, N., Martorell, M., & Cho,
W. C. (2020). Therapeutic Potential of Quercetin: New Insights and
Perspectives for Human Health. ACS omega, 5(20), 11849–11872. https://doi.org/10.1021/acsomega.0c01818
7. Suzuki, T., & Hara, H. (2011). Role of flavonoids in intestinal tight junction regulation. The Journal Of Nutritional Biochemistry, 22(5), 401-408. doi: 10.1016/j.jnutbio.2010.08.001
8.
Toth S, Jonecova Z, Curgali K, Maretta M, Soltes J. (2017). Quercetin
attenuates the ischemia reperfusion induced COX-2 and MPO expression in
the small intestine mucosa. Biomedical Pharmacotherapy. 95:246-254. https://www.ncbi.nlm.nih.gov/pubmed/28858733
TRIBUTYRIN
1.Cresci,
G. A., Glueck, B., McMullen, M. R., Xin, W., Allende, D., & Nagy,
L. E. (2017). Prophylactic tributyrin treatment mitigates chronic-binge
ethanol-induced intestinal barrier and liver injury. Journal of gastroenterology and hepatology, 32(9), 1587–1597. https://doi.org/10.1111/jgh.13731
2.
HM Hamer, D Jonkers, K Venema, S Vanhoutvin, FJ Troost, RJ Brummer.
Review article: the role of butyrate on colonic function. Alimentary
Pharmacology and Therapeutics. 2008, 27(104-119).
3.
Miyoshi, M., Iizuka, N., Sakai, S., Fujiwara, M., Aoyama-Ishikawa, M.,
Maeshige, N., Hamada, Y., Takahashi, M., & Usami, M. (2015). Oral
tributyrin prevents endotoxin-induced lipid metabolism disorder. Clinical nutrition ESPEN, 10(2), e83–e88. https://doi.org/10.1016/j.clnesp.2015.02.001
4.
Mortensen, P. B., & Clausen, M. R. (1996). Short-chain fatty acids
in the human colon: relation to gastrointestinal health and disease. Scandinavian journal of gastroenterology. Supplement, 216, 132–148. https://doi.org/10.3109/00365529609094568
5.
Murray, R. L., Zhang, W., Iwaniuk, M., Grilli, E., & Stahl, C. H.
(2018). Dietary tributyrin, an HDAC inhibitor, promotes muscle growth
through enhanced terminal differentiation of satellite cells. Physiological reports, 6(10), e13706. https://doi.org/10.14814/phy2.13706
6.
Ohira H, Fujioka Y, Katagiri C, Mamoto R, Aoyama-Ishikawa M, Amako K,
Izumi Y, Nishiumi S, Yoshida M, Usami M, Ikeda M. Butyrate attenuates
inflammation and lipolysis generated by the interaction of adipocytes
and macrophages. J Atheroscler Thromb. 2013;20(5):425-42.
7.
Roberto Berni Canani, Margherita Di Costanzo and Ludovica Leone. The
epigenetic effects of butyrate: potential therapeutic implications for
clinical practice. Clinical Epigenetics 2012, 4:4. http://www.clinicalepigeneticsjournal.com/content/4/1/4
8. Scheppach W. (1994). Effects of short chain fatty acids on gut morphology and function. Gut, 35(1 Suppl), S35–S38. https://doi.org/10.1136/gut.35.1_suppl.s35
9.
Singh, N., Thangaraju, M., Prasad, P,D., Martin, P,M., Lambert, N,A.,
Boettger, T., Offermanns, S., Ganapathy, V. (2010) Blockade of Dendritic
Cell Development by Bacterial Fermentation Products Butyrate and
Propionate through a Transporter (Slc5a8)-dependent Inhibition of
Histone Deacetylases. The Journal of Biological Chemistry. Sept 2010.
285: 36 (27601-27609). http://www.jbc.org/content/285/36/27601.full.pdf
10.
Tazoe, H., Otomo, Y., Kaji, I., Tanaka, R., Karaki, S. I., &
Kuwahara, A. (2008). Roles of short-chain fatty acids receptors, GPR41
and GPR43 on colonic functions. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 59 Suppl 2, 251–262.
11.
Wang, C., Cao, S., Zhang, Q., Shen, Z., Feng, J., Hong, Q., Lu, J.,
Xie, F., Peng, Y., & Hu, C. (2019). Dietary Tributyrin Attenuates
Intestinal Inflammation, Enhances Mitochondrial Function, and Induces
Mitophagy in Piglets Challenged with Diquat. Journal of agricultural and food chemistry, 67(5), 1409–1417. https://doi.org/10.1021/acs.jafc.8b06208
12.
Wang, C., Cao, S., Shen, Z., Hong, Q., Feng, J., Peng, Y., & Hu, C.
(2019). Effects of dietary tributyrin on intestinal mucosa development,
mitochondrial function and AMPK-mTOR pathway in weaned pigs. Journal of animal science and biotechnology, 10, 93. https://doi.org/10.1186/s40104-019-0394-x